When Is Lung Transplant Necessary for Pulmonary Hypertension?
Struggling with shortness of breath, fatigue, or swelling due to pulmonary hypertension (PH)? Pulmonary hypertension (PH) is a severe condition where the blood pressure in the arteries of the lungs becomes elevated, putting undue pressure on the heart. If left untreated, it can lead to heart failure and other life-threatening complications. In the most severe cases, a lung transplant for pulmonary hypertension may be considered as a final treatment option to improve quality of life and survival rates.
“A lung transplant is often the last resort when all other interventions fail to control PH,” says Dr. Prashant Bobhate, a distinguished pediatric cardiologist in Mumbai. “However, with timely diagnosis and intervention, many patients can avoid reaching that point.”
Dr. Prashant Bobhate has over a decade of experience in diagnosing and managing PH. He specializes in providing comprehensive care for PH patients, recommending lung transplant for pulmonary hypertension in Mumbai only when necessary, while focusing on interventional treatments and therapies to improve heart and lung function.
At Kokilaben Dhirubhai Ambani Hospital, Dr. Bobhate offers personalized, minimally invasive treatments aimed at improving quality of life and preventing severe outcomes, such as the need for a transplant.
Unsure what pulmonary hypertension exactly is? Let’s break down the condition and its impact on heart and lung function.
What is Pulmonary Hypertension?
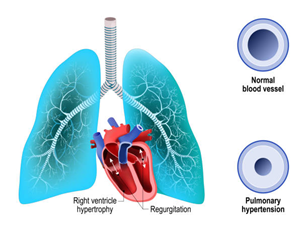
Pulmonary hypertension (PH) is a condition in which the blood vessels in the lungs become narrowed, making it harder for blood to flow through them. This leads to increased pressure in the pulmonary arteries and strains the right side of the heart.
As a result, the heart struggles to pump blood effectively to the lungs, leading to symptoms such as shortness of breath, fatigue, dizziness, chest pain, and swelling in the legs or abdomen. PH can be caused by various factors, including congenital heart defects, chronic lung diseases, or blood clots in the lungs.
Wondering if a lung transplant is the right option for PH? Let’s explore when this life-changing treatment becomes necessary.
When Is Lung Transplant Considered for PH?
Lung transplant is considered when pulmonary hypertension is severe and other treatments—such as medications, oxygen therapy, and minimally invasive procedures—no longer provide relief. This may include cases where PH has led to irreversible damage to the lungs or heart, or when there’s a significant decline in the patient’s ability to function normally.
Dr. Bobhate suggests considering transplant in the following scenarios:
Heart and lungs don't respond to medications or therapies anymore.
The patient has continual severe symptoms despite the treatment.
The patient's general condition is continuing to deteriorate, leading to a decline in the quality of their life.
Some other life-threatening complications develop due to PH
Let’s delve into the factors determining transplant eligibility in PH patients.
Eligibility Criteria for Lung Transplant

Severe Pulmonary Hypertension
Patients with PH that does not respond to medications or interventional treatments are typically considered for a lung transplant.
Age and General Health
Eligibility will be dependent on age and general health. Generally, patients can be considered if they are under 65 years of age and have good overall health excluding heart and lung issues.

Progressive Disease
Candidates often include patients in whom PH has progressed despite maximal medical therapy and in whom lung function continues to deteriorate.
No Severe Complications
Patients must have no active infections, cancer, or other serious medical conditions that would complicate the transplant.
Are there nonsurgical options prior to transplant? Let’s explore the alternatives available for the effective management of pulmonary hypertension.
Alternative Treatments Before Transplantation
Before considering a lung transplant, Dr. Bobhate typically pursues multiple minimally invasive PH treatment options that include the following:

Medications
Drugs like prostacyclins, endothelin receptor antagonists, and PDE-5 inhibitors promote the dilation of pulmonary blood vessels and thereby reduce pulmonary pressure.

Oxygen Therapy
Supplemental oxygen therapy is utilized to help ease breathing for patients with low oxygen levels, lessening stress on the heart and lungs.

Balloon Pulmonary Angioplasty
In chronic thromboembolic pulmonary hypertension (CTEPH) patients, balloon angioplasty can be used to open up narrowed pulmonary arteries.

Lung Volume Reduction Surgery
In certain cases, removing damaged lung tissue can improve lung function and help manage PH symptoms.
Thinking about the risks and advantages of a lung transplant for PH? Let’s evaluate both sides of this life-changing procedure.
Risks and Benefits of Lung Transplant
Risks
Improved Quality of Life
Lung transplant can significantly improve breathing, reduce symptoms, and allow for a more active lifestyle.
Increased Life Expectancy
A successful transplant offers patients the potential for many more years of life, often with better heart and lung function.
Benefits
Rejection of the New Lung
There’s always the risk that the body may reject the transplanted lung, requiring immunosuppressive therapy.
Infections and complications
Post-transplant, patients are at increased risk of infections, and the procedure itself carries inherent risks.
Ongoing Medications
Medications to prevent rejection of the organ and symptomatic controls should be taken throughout their lives, and most of them have side effects.
Let’s walk through the key stages of this life-saving procedure.
Lung Transplant Process Overview

Evaluation and Listing for Transplant
After a comprehensive evaluation, patients who meet the criteria are added to the transplant waiting list.
Donor Matching

The Surgery
Post-Operative Care
Post-surgery, the patient is under observation in the Intensive Care Unit. The post-transplant care consists of medication, monitoring, and rehabilitation that promote recovery.
Long-Term Follow-Up
This would include regular follow-ups, mainly for monitoring lung function, medication management, and prevention of complications such as organ rejection or infection.
Recovery and Long-Term Care

Initial Recovery
Post-surgery monitoring, pain management, and infection prevention are usually the reasons patients stay in the hospital for 1-2 weeks.
Physical Rehabilitation
Rehabilitation programs help patients regain strength and endurance, which can take several months.

Ongoing Monitoring
Regular follow-up visits are essential to track lung function, manage medications, and monitor for rejection or infections.
Lifelong Medication
Patients must take immunosuppressive medications for life to prevent rejection of the new lung.
Conclusion
Lung transplant can offer new hope for those with severe pulmonary hypertension who have exhausted other treatment options. Timely intervention, expert care, and a structured approach are critical for a successful outcome.
Dr. Prashant Bobhate offers advanced, effective treatment for pulmonary hypertension in both adults and children. His personalized approach ensures that each patient receives the most suitable treatment, whether through medications, minimally invasive procedures, or a transplant.
FAQs
1. When should a lung transplant be considered for PH?
When PH is severe and other treatments fail to improve symptoms or quality of life, a lung transplant is considered.
2. How long does the recovery take after a lung transplant?
Initial recovery takes 1-2 weeks in the hospital, with full recovery and rehabilitation taking several months.
3. What is the survival rate after a lung transplant?
The survival rate varies but many patients live for many years after a successful transplant with proper care.
4. Can pulmonary hypertension be managed without a lung transplant?
Yes, with medications, oxygen therapy, and other interventions, PH can often be managed without the need for a transplant.
5. Can lung transplant be done for children with PH?
Yes, if the child is in critical condition when other treatments don’t work then lung transplantation is considered.
Disclaimer: The information shared in this content is for educational purposes and not for promotional use